Our Adventure Therapy program immerses you in some of Maui’s most pristine natural settings. These exhilarating experiences offer our clients a unique opportunity to make a life-saving “shift” towards lasting recovery.
Why Maui Recovery Stands Out For Adventure Therapy in Hawaii
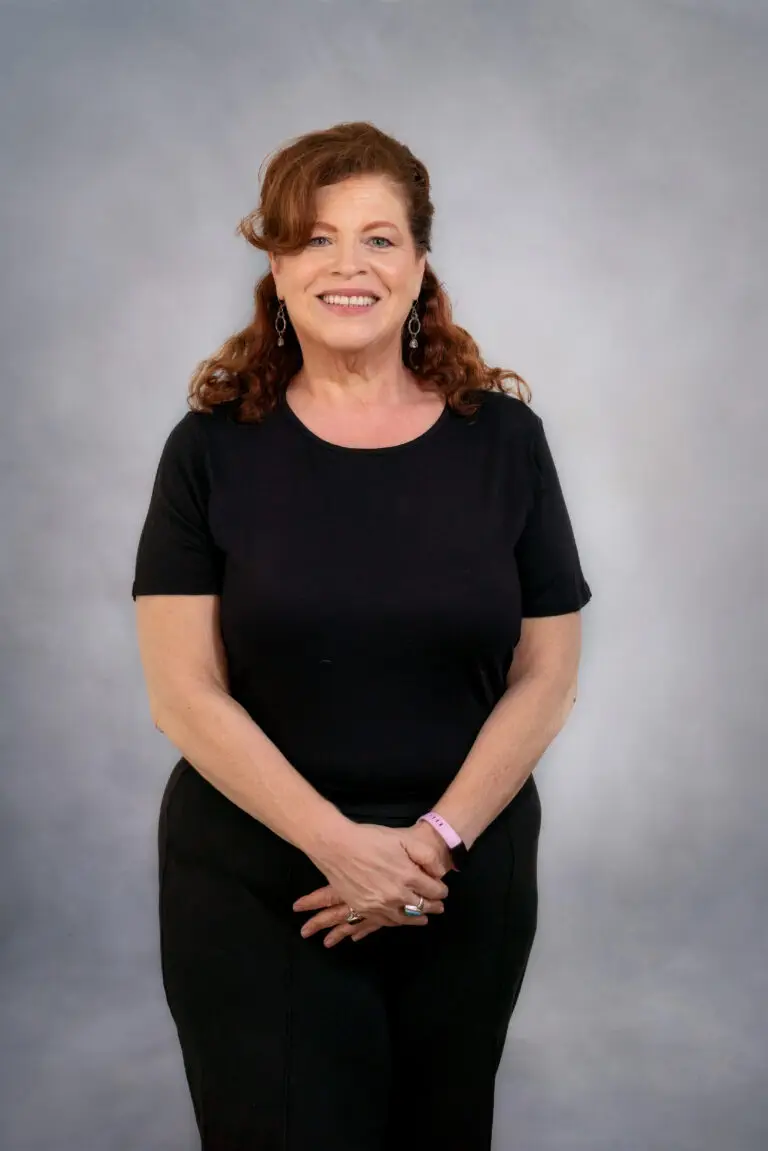
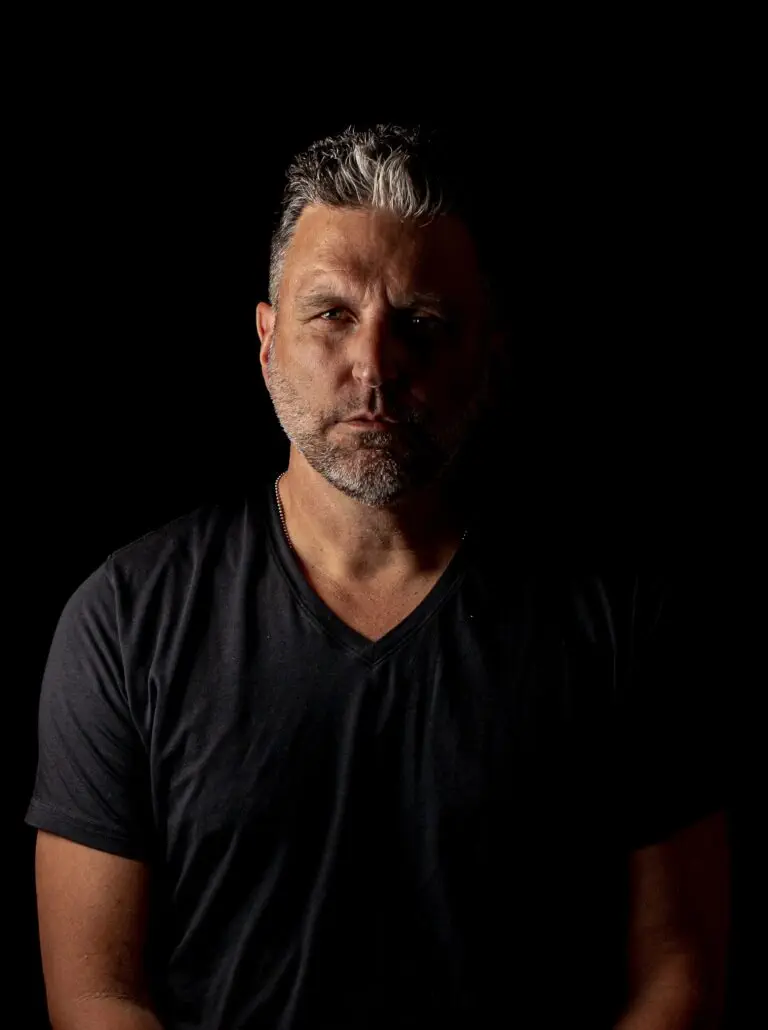
Our team of therapists and addiction recovery experts aren’t just professionals—they’re compassionate mentors dedicated to guiding you through every phase of your journey. With their wealth of experience, genuine care, and empathetic support, they create an optimal environment for healing, personal growth, and long-term recovery. Here are some of the key aspects of our outdoor therapy program:
Transformative Outdoor Adventures
Dive into the vibrant depths of Molokini Crater while snorkeling or trek through the lush landscapes of Iao Valley on one of our Adventure Therapy excursions. These experiences harness the power of nature to inspire change, challenge your limits, and unearth inner strengths essential for lasting transformation.
Transformative Outdoor Experiences
From snorkeling in the vibrant Molokini Crater to hiking through the lush Iao Valley, our Adventure Therapy programs use the power of nature to inspire change. Our adventures are designed for clients ready to face challenges, discover inner strengths, and experience lasting transformation.
Distinctive Hawaiian Setting
Immerse yourself in Maui’s natural splendor, where tranquil turquoise waters meet lush landscapes, creating a tropical haven ideal for reflection and rejuvenation. The island’s diverse marine life and breathtaking vistas offer a serene backdrop for your recovery journey.
Holistic Healing Approach
At Maui Recovery, we believe in addressing the entirety of the individual—not just the addiction. Our holistic programs seamlessly integrate physical, emotional, and spiritual healing modalities, ensuring a comprehensive and personalized recovery experience tailored to your unique needs.
Culturally Enriching Activities
Embrace the rich tapestry of Hawaiian culture through immersive experiences like outrigger canoeing, where you’ll delve into Maui’s history and forge a deeper connection with its spirit. These culturally immersive activities foster a greater understanding of yourself and the world around you, enriching your recovery journey with newfound insights and perspectives.
Exciting Adventures Await You in the Hawaiian Outdoors
Snorkel in Turtle Town

The calm, crystalline waters of Turtle Town are the perfect place to observe the natural habitat of the majestic and endangered Hawaiian Green Sea Turtles. These gentle giants, which can grow up to four feet and weigh up to 400 pounds, glide gracefully among the underwater lava formations and rich marine life.
Discover the Molokini Crater
Maui’s Molokini, a crescent-shaped, submerged volcanic crater, is filled with vibrant marine life and colorful tropical fish. The unique crater provides a natural shield from strong currents and waves and is an ideal spot for both beginner snorkelers to discover the underwater wonders of Molokini.
Explore Turtle Reef
Dive into one of Maui’s premier snorkeling destinations with a vibrant underwater sanctuary of (completely harmless!) manta rays and black-tip nurse sharks. Beyond the captivating marine life, Turtle Reef boasts impressive coral formations, with some larger coral heads being hundreds of years old.
Hike to Twin Falls

Situated along the iconic Road to Hana, Twin Falls is a must-visit attraction and a perfect example of the island’s diverse beauty. A moderate hike into the lush forest culminates with the majestic Twin Waterfalls. Take a dip and relax in the deep pools, surrounded by vibrant foliage and unique natural wonders, all nurtured by the frequent rains in the Ho’olawa Valley.
Journey Through Iao Valley
Located along the central plains of Maui is the unmistakable pinnacle of the ‘Iao Needle’, 1,200 feet above the valley floor—a striking green-hued remnant from West Maui’s last eruption over 320,000 years ago. A short hike is richly rewarded with panoramic views of expansive valleys, dramatic ridges, and the shimmering coastline. The breathtaking beauty of this National Natural Landmark led Mark Twain to affectionately call it the “Yosemite of the Pacific.”
Experience Outrigger Canoeing

Quintessential symbols of Hawaii, traditional outrigger canoes have been part of Hawaiian culture since 200 AD. Today, they serve diverse purposes, from whale watching to racing competitions. If you’re ready to immerse yourself in marine life, history, and culture, Maui Recovery offers an authentic outrigger canoeing experience, combining a thrilling ocean adventure with fascinating information about endemic marine life and Hawaiian culture.
Bike in Makawao Forest
The serene Makawao Forest, a hidden gem nestled in the heart of Maui reminiscent of the enchanting landscapes described by John Muir. The misty, bird-song-filled trails, 3,000 feet above sea level, make it a haven for biking adventures. Meandering alongside a gorge and winding its way through a verdant forest of vibrant flora, the primary path of the Kahakapao Loop Trail reveals an opportunity to experience the restorative power of nature.
Why Choose Adventure Therapy Through Maui Recovery?
Adventure therapy provides a range of benefits that contribute to holistic well-being and personal growth. Engaging in outdoor activities such as hiking, rock climbing, or kayaking promotes physical health by improving fitness, muscle strength, flexibility, and endurance.
Explore Behind Your Comfort Zone – Participating in these activities encourages individuals to step outside their comfort zones, confront challenges, and develop emotional resilience and coping skills. The calming effects of natural environments can reduce stress levels, lower anxiety, and improve mood, leading to a greater sense of well-being.
Foster a connection with the outdoors – Adventure therapy offers opportunities for individuals to connect with the natural world, fostering feelings of awe, wonder, and appreciation for the environment. Building connections with others in group-based adventure activities promotes teamwork, communication, and collaboration, enhancing social skills and interpersonal relationships.
Encourage Personal Growth – Engaging in outdoor adventures challenges individuals to confront fears, take risks, and explore new possibilities, facilitating personal growth and development. Ultimately, adventure therapy offers moments of joy, excitement, and fulfillment, cultivating a sense of playfulness, spontaneity, and creativity that enhances overall quality of life.
Join Us on the Road to Recovery
At Maui Recovery, we offer more than just a treatment program; we provide transformative Adventure Therapy experiences that redefine the journey to recovery. Surrounded by the healing powers of nature and guided by a team dedicated to your success, you’ll find the strength, courage, and serenity to overcome addiction and rediscover joy. Are you ready for a life filled with adventure, healing, and hope? Contact us today and discover a new chapter in your life.

Your recovery awaits
Meet our team